Information
This section covers everything you need to know about intrahepatic cholestasis of pregnancy (ICP) during pregnancy, labour and after the birth of your baby.
We are the UK’s only dedicated research-based charity for ICP. All the information we provide is based on the most up-to-date academic research.
If you find the information here helpful, why not make a donation so that as a charity we can continue to help fund research?
-
SUMMARY
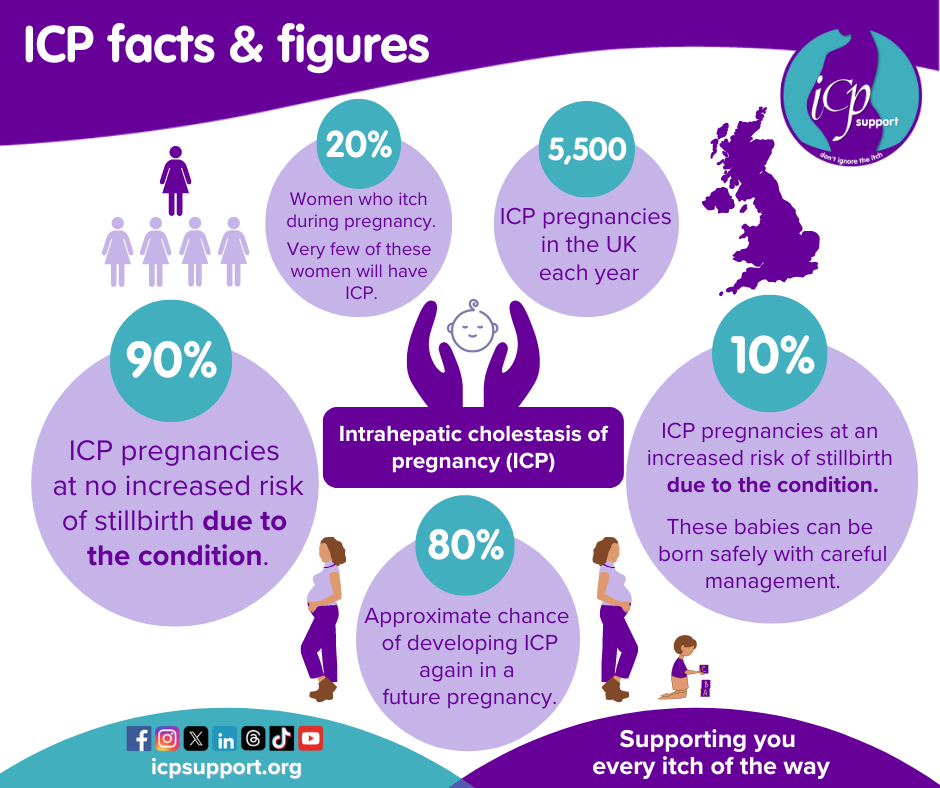
Intrahepatic cholestasis of pregnancy (ICP), also known as obstetric cholestasis (OC), is the most common pregnancy-specific liver condition. It has an incidence in the UK of 0.7% (affecting around 5,500 women and birthing people a year). British South Asian women have almost twice the incidence. It is more common in other parts of the world – around 5% in South America and 2% in Scandinavia.
ICP occurs when the flow of bile, which is produced in the liver and stored in the gallbladder, becomes sluggish. The bile acids in bile help us to digest food, but they are toxic in large amounts. As the flow of bile slows down, these bile acids build up and flow back into the bloodstream. They are not life-threatening for the mother-to-be, but research has shown that they cross the placenta and may affect the baby’s heart.
ICP is associated with premature labour, fetal distress and, in severe cases, stillbirth. More recently, research has shown women who have had ICP may go on to develop liver disease.
More detailed information about:
– SYMPTOMS
– CAUSES -
SUMMARY
The diagnosis of ICP will usually involve blood tests and doctors may also want to exclude other causes of itch. The two blood tests commonly performed include a total bile acid test (which should always be a non-fasting test) and a liver blood test (also called a liver function test). If your first bile acid test comes back as normal (under 19 µmol/L) but you continue to itch, it is important that you continue to be tested, as research shows that some people can itch for many weeks (up to 15 weeks) before the bile acid levels become abnormal.
There is no cure for ICP, but the condition should resolve once you have your baby. Once diagnosed, management of the condition will typically include treatment where appropriate (such as ursodeoxycholic acid, which has been shown to have benefits when bile acids are >40 µmol/L) and regular blood tests (bile acids and liver blood tests). You may also be asked to have a liver ultrasound scan. Many hospitals will use CTGs (cardiotocographs) or NSTs (non-stress tests) to check your baby’s heart rate, but these have not been found to be of any benefit in detecting problems for your baby in ICP. The birth of your baby will be based on how high your non-fasting bile acids rise; a concentration of >100 µmol/L is when the risk of stillbirth occurs (3.44%) and means that your baby is likely to need to be born around 35 weeks of pregnancy. If your bile acids always remain <100 µmol/L it is possible that you could wait to meet your baby as late as 40 weeks of pregnancy.
More detailed information about diagnosis and management can be found by clicking the links below:
– DIAGNOSIS
– TREATMENT AND MANAGEMENT
– MANAGEMENT GUIDELINES -
SUMMARY
The cause of stillbirth in ICP is associated with high non-fasting bile acid concentrations (3.44% when total non-fasting bile acids are over 100 µmol/L). The liver enzymes measured in the liver blood test are not linked to stillbirth in ICP alone. The risk of stillbirth when concentrations are over 100 µmol/L is reduced by inducing the birth of your baby around 35 weeks of pregnancy. Most women with ICP (90%) will never have bile acids over 100 µmol/L, which means that their risk of stillbirth is no different from those women who have no pregnancy complications.
More detailed information about risk can be found by clicking the link below: -
SUMMARY
When you have your baby may depend on how high your non-fasting bile acids have risen, and you may be able to wait until 38–40 weeks for induction if your bile acids always remain <100 µmol/L. But this may also depend on how you are coping with your itching. The psychological impact of ICP can never be underestimated, especially if your itch is very severe, and you may find that even though your bile acid results mean you could wait until 40 weeks, the prospect of coping with the itch for that long is just too much for you. You can discuss this with your doctor – never be afraid to let them know just how badly the condition is affecting you, both physically and psychologically.
Where you give birth may also depend on your bile acids but could include birth centres, which are more like home-from-home wards rather than labour wards, or a midwifery-led unit. If your hospital provides these services do talk to them about this. It may be possible to have a homebirth if your bile acids always remain <40 µmol/L but you will need to discuss this with your health professionals.
More detailed information on this can be found by clicking the link below:
-
SUMMARY
Recent research has shown that some women who have had ICP have a higher chance of developing liver disease, so it is important that your bile acids and liver enzymes all return to normal after ICP.
Contraception involving hormones needs to be carefully considered, and HRT can also be used.
More detailed information on this can be found by clicking the link below: -
Downloadable leaflets in various languages containing the essential information about ICP.
-
Helpful research papers for you to download
Next > Symptoms